Systemic Lupus Erythematosus and Nursing

After 30 years of being in the nursing field, I have witnessed so much from tears of joy to despair. I have witnessed people being told they only had 3 months to live, and then they defy all odds and recover.
Therefore, when I care for a patient with systemic lupus erythematosus or SLE, my heart truly aches. Don’t misunderstand me.
My heart aches because they are some of the sweetest patients, and they have his challenging disease.
What is Systemic Lupus Erythematosus?
Systemic lupus erythematosus (SLE), is the most common type of lupus.
SLE is an autoimmune disease in which the immune system attacks its own tissues, causing widespread inflammation and tissue damage in the affected organs.
It can affect the joints, skin, brain, lungs, kidneys, and blood vessels.
There is no cure for lupus, but medical interventions and lifestyle changes can help control it.
The cause of SLE is unknown. However, it is thought to be caused by a combination of environmental, genetic, or hormone factors.
Systemic lupus erythematosus (SLE), can be from mild to life-threatening. With good treatment, a person with SLE can have a good quality of life.
Systemic Lupus Erythematosus and Nursing
SLE can be pretty difficult to diagnose because sometimes the symptoms mimic other disorders. Often when I work in the emergency department, these patients come in, they present like kidney or heart patients.
I suppose, in reality, these patients do present like heart and kidney patients because these two organs are the most affected by SLE.
Muscle and joint pain:
This is one of the hallmark symptoms of SLE. People start having muscle and joint pain. Often time it is mistaken for arthritis or “getting old”. People sometimes describe it as ” a burning pain”.
When patients go see their doctors, the doctors don’t immediately think of SLE or lupus because it is a rare disorder. The doctors will prescribe Motrin and send them about their way.
Fever:
Fever is another common symptom. Everyone gets a fever when they have a cold or if they have an infection brewing. In fact, most people do not go to the doctor if they “just” have a fever. In lupus, the fever is from inflammation.
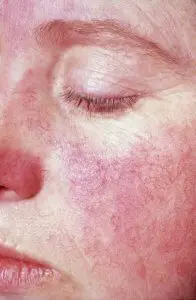
Rashes:
Another hallmark symptom of lupus is the “lupus rash”. Often times people assume the rash is from the sun. For some unknown reason, people who have lupus can’t tolerate the sun. I have heard people with an unknown diagnosis if lupus says, ” I just cannot tolerate the sun, or the sun makes me sick.

Chest pain:
Although chest pain is not a common symptom of lupus, it can happen. Lupus is a “younger” woman disease. Therefore, when patients come into the hospital for chest pain, doctors rarely think of lupus. Lupus does attack the lining of the heart and causes inflammation. As a result, you will have chest pain.
Hair loss:
Hair loss is probably caused by inflammation and nutrient loss. Let’s face it, a woman’s hair is her glory and when a woman loses her hair it can be devastating.
Sun sensitivity:
Besides the rash, sun sensitivity is one of the main symptoms that alert patients that something is wrong. Although sometimes medication can have this effect. It seems as if the person is in a sauna. Their skin actually burns.
Putting on sunscreen does not help.
Related Articles
Whol medical abbreviation
What is TKO?
What is an RNC?
Parkinson Nursing Care Plan
Kidney problems:
Lupus affects the kidneys because lupus attacks the kidney cells and it causes a disorder called lupus nephritis. The sun exposure can cause joint pain, muscle pain, and eye pain.
Blood clotting problems: Inflammation can sometimes cause blood clotting issues. Blood clots are dangerous because if a clot gets into your heart or lungs, it can be dangerous.
How Do You Know If You Have Lupus
Now that you have read all about the symptoms of SLE, how do you know if you have lupus?
SLE is diagnosed by a health care provider using symptom assessments, physical examination, X-rays, and lab tests.
SLE may be difficult to diagnose because its early signs and symptoms are not specific and can look like signs and symptoms of other diseases.
SLE may also be misdiagnosed if only a blood test is used for diagnosis. Because diagnosis can be challenging, it is important to see a doctor specializing in rheumatology for a final diagnosis. (Source).
SLE and Nursing Care
Lupus patients are usually younger, therefore they usually have “younger” children. Nursing care of the lupus patient involves the entire family.
I recall caring for a lupus patient years ago. She was diagnosed only 18 months earlier, but she was so sweet. She had 3 children under the age of 18. However, she was suffering from kidney problems, liver problems, and heart problems.
She frequently had nausea and vomiting. Because of the liver failure, she developed fluid or ascites in her belly, and it has to be removed every two weeks.
The fluid in her belly made her look like she was 9 months pregnant. She was so uncomfortable,
As her nurse, I was charged with being her advocate and to make sure that she was very comfortable.
I knew her belly was sore because she had a paracentesis earlier in the day. A paracentesis is a procedure where the doctor withdraws fluid out of your abdomen. The procedure does not hurt and it makes the patient feel so much better.
How Should a Nurse Assess a Lupus patient?
When a nurse is assessing a patient with lupus, there are several important things to look for in order to provide comprehensive care and support. Lupus is an autoimmune disease that can affect various parts of the body, so a thorough assessment is crucial. Here are the key aspects to focus on:
- Medical History and Symptoms: Start by gathering the patient’s medical history, including any previous diagnoses, medications, and surgeries. Ask about their current symptoms, such as joint pain, fatigue, skin rashes, and sensitivity to sunlight. Pay attention to the frequency, severity, and duration of these symptoms.
- Skin and Joints: Examine the patient’s skin for any visible rashes, which can be a hallmark of lupus. The classic “butterfly rash” on the face is common. Assess joints for tenderness, swelling, and limited range of motion, as lupus can cause arthritis-like symptoms.
- Vital Signs: Measure the patient’s vital signs, including blood pressure, heart rate, respiratory rate, and temperature. Monitoring these parameters helps track any potential complications or changes in their health status.
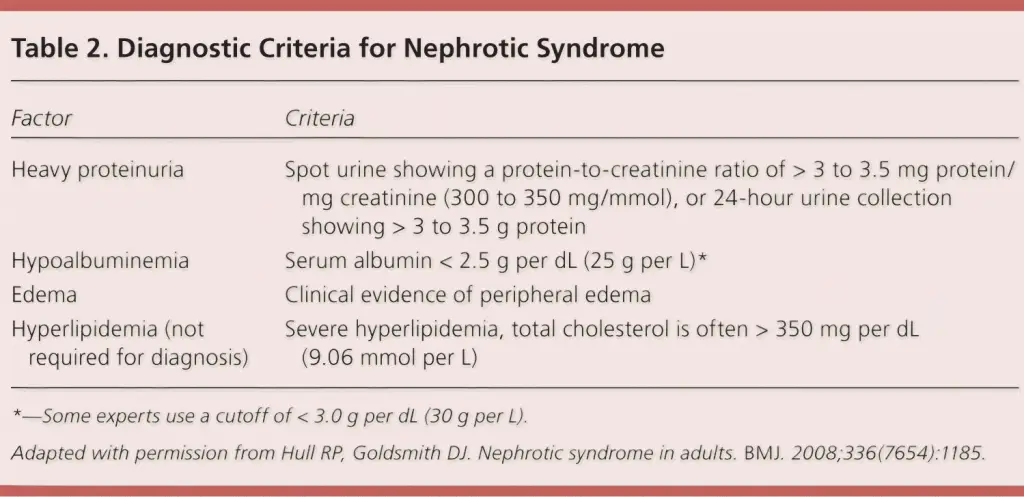
- Renal Function: Lupus can affect the kidneys, so it’s important to assess renal function. Check for signs of kidney involvement such as edema (swelling), changes in urine output, and blood in the urine. Monitoring kidney function through laboratory tests is also essential.
- Cardiopulmonary Assessment: Evaluate the patient’s heart and lungs. Lupus can cause inflammation in these organs, leading to chest pain, shortness of breath, and irregular heartbeats. Listen to lung and heart sounds and monitor for any abnormalities.
- Neurological Assessment: Perform a neurological assessment to check for symptoms like headaches, cognitive difficulties, and numbness or weakness in extremities. Lupus can affect the nervous system, causing various neurological manifestations.
- Gastrointestinal Evaluation: Some patients with lupus might experience gastrointestinal issues like abdominal pain, nausea, and vomiting. Inquire about any digestive symptoms and assess the abdomen for tenderness or distention.
- Mental and Emotional Health: Lupus can have a significant impact on mental and emotional well-being. Ask the patient about their mood, anxiety, and any cognitive changes. Be prepared to provide resources or referrals for psychological support if needed.
- Medication Review: Review the patient’s current medications, including prescribed medications for lupus and any other conditions. Ensure they are taking medications as prescribed and monitor for potential drug interactions or side effects.
- Educational Support: Take the time to educate the patient about lupus, its potential complications, and strategies for managing their condition. Provide resources for further information and self-care.
Remember, a comprehensive assessment involves not only gathering information, but also actively listening to the patient’s concerns and addressing their questions. Communication and empathy are essential in providing holistic care to individuals with lupus.
Nursing Interventions for the Lupus Patient
- It is extremely important to do a thorough assessment. We have to remember that the doctor is not with the patient 24 hours a day. The nurses are with the patient 24 hours a day.
- Pain control is extremely important for the lupus patient. This is important to remember: only the patient knows if he is in pain. Please do not hold the patient’s medication. Of course, if there is a contraindication, the pain meds should be held.
- Although the doctors are responsible for ordering lab work, the nurse should be checking the patient lab results for the blood count and clotting factors level.
- Accurate intake and output are important because of the kidney involvement that the majority of lupus patients has.
- Psychosocial support is important because these are usually younger, female patients with families. Sometimes they are depressed, angry, and sad. These are all emotions that you will see as a nurse and as a family member.
- Don’t forget the families. They need support too. It is good practice to ask the patient if they would like to see the chaplain.
There is no cure for SLE. The treatments are used to support the patients quality of life. One of the main treatments is steroids. Steroids can lead to diabetes. Therefore, patients and nurses should be monitoring sugar levels.
Many lupus patients are on dialysis because of the kidney problems that lupus is infamous for.
Heart failure is another complication of lupus. Heart failure is treated by medications, diet and lifestyle changes.
Conclusion
There are several books that are recommended for the lupus patient. These books are listed below.
Lupus can be managed with excellent treatment and lifestyle changes. Nurses play an important role in making sure the lupus patient is made as comfortable as possible.
Do you have lupus? Leave me a comment on how you are managing your disorder.
Related Articles
Nursing care plan for congestive heart failure
Nursing Diagnosis Care Plan For Parkinson Disease
Why do veins roll?
Phyllis Robinson MSN, RN is a Registered Nurse of 27 years. Phyllis is passionate about the prevention and healing of heart disease using traditional and alternative methods. She has experience in emergency room, telemetry, infusion, and critical care. Phyllis currently practices in an intensive care unit.