Nursing Care Plan for Patients with Parkinson’s Disease
Parkinson’s disease is a chronic and progressive neurological disorder that affects a person’s ability to move and control their movements.
It is caused by the degeneration of dopaminergic neurons in the brain, which leads to a deficiency in the neurotransmitter dopamine.
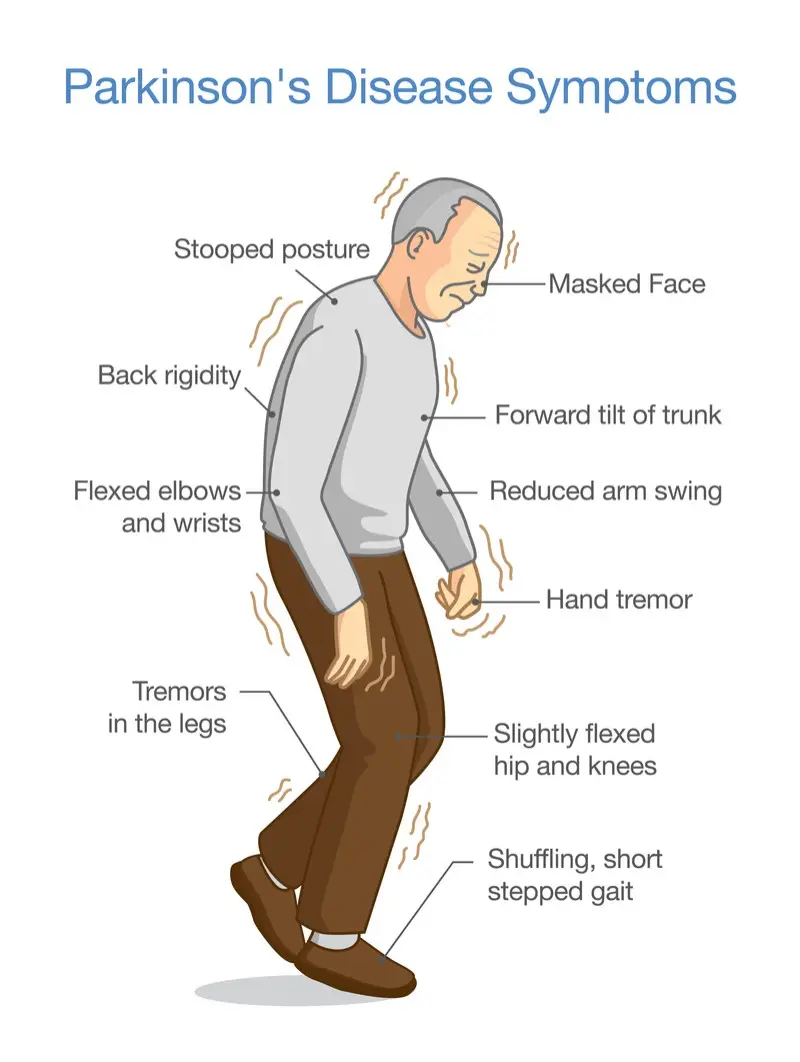
This deficiency results in the characteristic motor symptoms of Parkinson’s disease, including tremors, rigidity, bradykinesia (slowness of movement), and postural instability.
As Parkinson’s disease progresses, patients may also experience non-motor symptoms, such as cognitive impairment, depression, and sleep disturbances.
These symptoms can significantly impact a patient’s quality of life, and as a result, nursing care plans for patients with Parkinson’s disease should address both the motor and non-motor symptoms of the disease.
Related Articles
What Can Nurses Claim on Income Tax
Assessment
Before developing a nursing care plan for a patient with Parkinson’s disease, it is important to conduct a thorough assessment of the patient’s current symptoms, functional abilities, and overall health status.
This assessment should include a review of the patient’s medical history, a physical examination, and an evaluation of the patient’s cognitive and psychological status.
Motor symptoms
Assessment of the patient’s motor symptoms should include an evaluation of their gait, balance, posture, and coordination.
The nurse should observe the patient’s movements and note any tremors, rigidity, or bradykinesia.
The nurse should also assess the patient’s ability to perform activities of daily living (ADLs), such as dressing, grooming, and feeding, as well as their ability to engage in leisure activities and hobbies.
Non-motor symptoms
Assessment of the patient’s non-motor symptoms should include an evaluation of their cognitive and psychological status. The nurse should assess the patient’s memory, attention, and executive functioning, as well as their mood and affect.
The nurse should also inquire about the patient’s sleep habits and any other non-motor symptoms they may be experiencing, such as constipation or urinary incontinence.
Nursing Diagnosis
Based on the assessment findings, the nurse should formulate nursing diagnoses that address the patient’s specific needs. Nursing diagnoses for patients with Parkinson’s disease may include:
- Impaired physical mobility related to tremors, rigidity, and bradykinesia
- Risk for falls related to postural instability
- Impaired self-care related to difficulty with ADLs
- Impaired social interaction related to depression or cognitive impairment
- Disturbed sleep pattern related to sleep disturbances
Planning
Once the nursing diagnoses have been identified, the nurse can develop a nursing care plan that addresses the patient’s specific needs.
The nursing care plan should be individualized to the patient and should include both short-term and long-term goals.
Short-term goals
Short-term goals should be achievable within a few days to a week and should focus on addressing the patient’s immediate needs. Examples of short-term goals for patients with Parkinson’s disease may include:
- Increase the patient’s ability to perform ADLs independently
- Improve the patient’s balance and reduce their risk for falls
- Reduce the patient’s tremors and rigidity through medication management and/or physical therapy
Long-term goals
Long-term goals should be achievable within weeks to months and should focus on improving the patient’s overall health and quality of life. Examples of long-term goals for patients with Parkinson’s disease may include:
- Improve the patient’s overall physical mobility and ability to engage in leisure activities
- Improve the patient’s cognitive functioning and reduce their risk for dementia
- Address the patient’s non-motor symptoms, such as depression and sleep disturbances
Interventions
The nursing interventions included in the care plan should be based on the identified nursing diagnoses and should be aimed at achieving the short-term and long-term goals. Interventions for patients with Parkinson’s disease may include:
- Promoting physical activity and mobility: The nurse should encourage the patient to engage in physical activity and exercise to improve their mobility and reduce the risk of falls. The nurse can work with a physical therapist to develop an exercise plan that is tailored to the patient’s needs and abilities.
- Medication management: The nurse should work with the patient’s healthcare provider to manage their medication regimen. The nurse should ensure that the patient is taking their medication as prescribed and should monitor for any adverse effects.
- Assistive devices: The nurse can recommend the use of assistive devices, such as canes or walkers, to improve the patient’s mobility and reduce their risk of falls.
- Education: The nurse should educate the patient and their family members about Parkinson’s disease and its management. This education should include information about the disease process, medication management, and strategies for managing motor and non-motor symptoms.
- Supportive care: The nurse should provide emotional and psychological support to the patient and their family members. This may include counseling or referral to support groups for patients with Parkinson’s disease.
- Environmental modifications: The nurse can make recommendations for modifications to the patient’s environment to reduce their risk of falls. This may include installing grab bars in the bathroom or removing tripping hazards from the home.
Evaluation
The nursing care plan should be regularly evaluated to determine its effectiveness in achieving the identified goals.
The nurse should assess the patient’s progress toward their goals and adjust the care plan as needed. The nurse should also monitor for any adverse effects of the interventions included in the care plan.
Conclusion
Parkinson’s disease is a chronic and progressive neurological disorder that can significantly impact a patient’s quality of life.
Nursing care plans for patients with Parkinson’s disease should be individualized to the patient’s specific needs and should address both the motor and non-motor symptoms of the disease.
Effective nursing interventions for patients with Parkinson’s disease include promoting physical activity and mobility, medication management, the use of assistive devices, education, supportive care, and environmental modifications.
Regular evaluation of the nursing care plan is essential to determine its effectiveness and adjust the plan as needed to achieve the identified goals. By implementing a comprehensive nursing care plan, nurses can help improve the quality of life of patients with Parkinson’s disease and their families.
Phyllis Robinson MSN, RN is a Registered Nurse of 27 years. Phyllis is passionate about the prevention and healing of heart disease using traditional and alternative methods. She has experience in emergency room, telemetry, infusion, and critical care. Phyllis currently practices in an intensive care unit.